CLINICAL EVIDENCE
Millions of in vitro diagnostic tests (IVDs) are performed every day to rule out, detect, confirm, and manage diseases and conditions. While much of what is usually seen from IVDs is little more than sample containers, test tubes, transport boxes and perhaps high-end analyzer machinery, it is good to remember that a report from an IVD diagnostic test – be it performed at the bedside, in the hospital lab, or in molecular biology central lab – is just the tip of the iceberg of innovative science, quality control and logistics translated into daily answers.
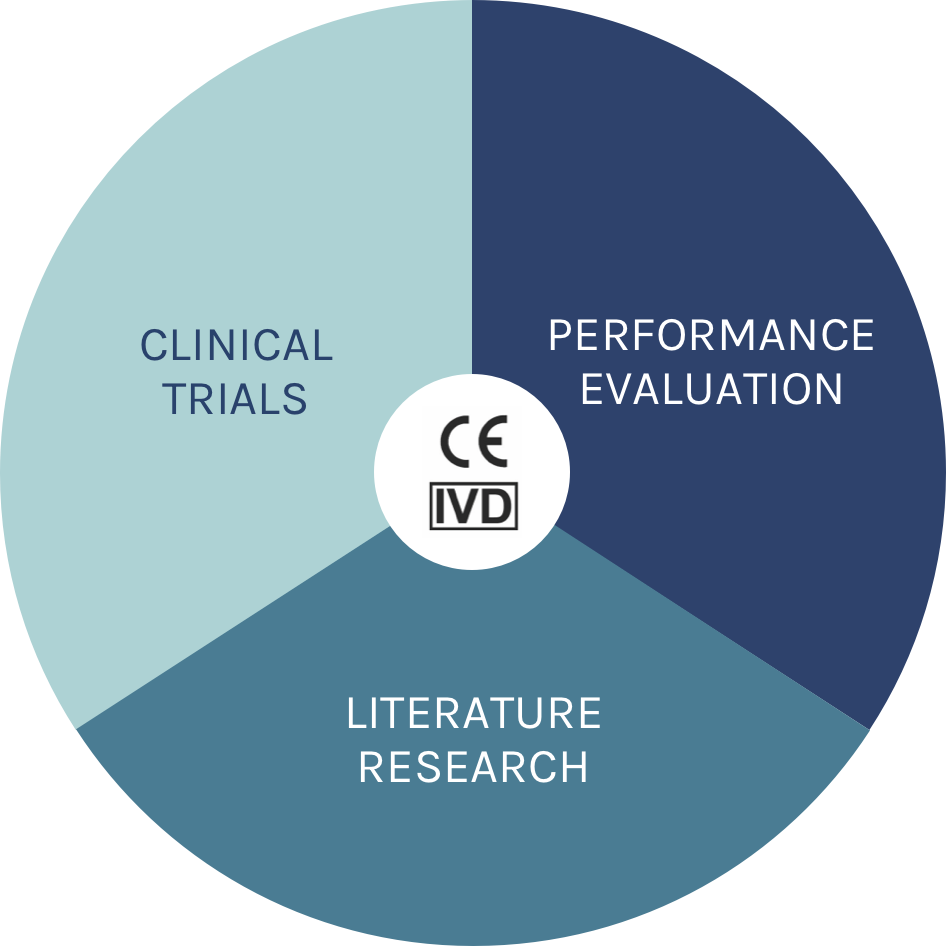
To safely provide these answers, IVDs are heavily regulated by the EU and member states. The CE-mark certification process for every IVD has hence to be conclusive regarding its scientific validity, analytical validity and clinical performance. No IVD test will have a CE-IVD mark unless it meets these demands for clinical evidence.
In other words, clinical evidence is always the sum of clinical trials + literature research + clinical performance = CE-IVD.
INDITREAT® IS AN IVD TEST, AND THEREFORE SUPPORTED BY CLINICAL EVIDENCE
After 14 years of research and development to improve the care for patients with mCRC, the IndiTreat® test is the first CE-IVD marked drug sensitivity test using three-dimensional tumoroids. Tumoroids are derived from fresh samples of colorectal cancer (CRC) tissue that has been obtained from an individual patient’s metastatic colorectal cancer.
IndiTreat® determines tumoroid growth inhibition by exposing many hundreds of these mini tumors in vitro to approved antineoplastic drugs and provides the treating oncologist with growth inhibition rates for each of the approved medications that come in question according to standard of care.
We will look at the three areas for IndiTreat®.
Performance Evaluation
The aim of the Resistance study [1] was to retrospectively compare a similar group of chemonaive control patients with mCRC to TICC-1 [2] trial patients who were regarded as clinically non-responding to FOLFOX, FOLFIRI and FOLFOXIRI. For each of the chemonaive control group patients, an IndiTreat® test was performed per usual test procedures on hundreds of tumoroids derived from individual tumor tissue as described above. The statistical analysis of any growth inhibition differences was performed using the appropriate Mann-Whitney test with a confidence level of 95% at α = 0.05; i.e. p-values below 0.05 were considered statistically significant.
For all three regimens, IndiTreat® results expressed as gradual growth inhibition of tumoroids from chemoresistant TICC-1 patients were significantly inferior compared to chemonaive control (all p <0.0004). 81%-94% chemoresistant patients showed LOW growth inhibition per IndiTreat® (FOLFIRI 94%, FOLFOX 81% and FOLFOXIRI 82%). Conversely, for chemonaive patients, 88%-100% of the patients presented HIGH growth inhibition per IndiTreat® (FOLFIRI 88%, FOLFOX 100% and FOLFOXIRI 100%), documenting the test’s ability to classify treatment responsiveness versus clinically resistance to the tested regimens at or surpassing the strict regulatory thresholds for CE-marked IVDs.

Literature Research
Systematic reviews of peer-reviewed data must consider, compile and report not only third-party peer-reviewed clinical information, but also technical, scientific and safety information from the technical family of products in use in the target population. This depends on the IVD test’s type of technology and on the clinical risk its application by user and the intended use entails.
IndiTreat® tests are cutting-edge among state-of the art 3D microtumor testing technology (organoids and tumoroids) in human cancers. Over 40 individual publications have been selected and described in detail. A recent review paper by Wensink et al. (2021) [3] has provided a pooled analysis of results regarding the use of patient-derived 3D microtumors in individualized tumor response testing, focusing on peer-reviewed evidence for analytical validity, clinical validity and clinical utility. Using 3D microtumors, predictive drug sensitivity results were obtained in clinical settings for 5-FU, FOLFOX and FOLFIRI, regorafenib and TAS102. There is no literature data on the clinical predictiveness of the treatment FOLFOXIRI, but FOLFOXIRI is a combination of FOLFOX and FOLFIRI.
Wensink et al. concluded that there is strong evidence that a large number of colorectal cancer patients show a correlation between drug
sensitivity screen results and systemic therapy.
Clinical Trials
The TICC-1 study [2] was a prospective interventional clinical trial conducted in a group of late-stage metastatic colorectal cancer (mCRC) patients with prior exposure to or intolerance/contraindications to standard systemic therapy (defined as oxaliplatin, irinotecan, 5-fluorouracil or similar such as capecitabine, bevacizumab, and if indicated panitumumab or cetuximab), and documented evidence of progression per Response Evaluation Criteria in Solid Tumors (RECIST 1.1.)
To define clinically relevant success criteria for IndiTreat® in TICC-1, it had to be considered that large last-line randomized trials in comparable late-stage populations reported only ca. 20% Progression Free Survival at the first evaluation (Grothey 2013; Mayer 2015) [4,5]. Hence, following good practice for generating diagnostic IVD clinical evidence, for the TICC-1 study a far higher Progression Free Survival (PFS) threshold of 40% at two months following IndiTreat® guidance was predefined. The TICC-1 study met its primary endpoint successfully, not only surpassing the challenging threshold, but more than doubling the historical 20% PFS rate [4,5] : TICC-1 results showed that with therapies following IndiTreat® test results, PFS at two months was found in an astonishing 50% of evaluable patients.
CONCLUSION
Only IVDs which fulfill all of the above requirements may be put on the market and be used by health care providers. Having met these complex regulatory provisions, therefore demonstrating sufficient clinical evidence, IndiTreat® is now being translated into clinical use across Europe. The ever-increasing pool of real-world data regarding 3D microtumor-based testing with IndiTreat® will support the clinicians’ decision making process for therapies in mCRC patients with severe medical needs.
References
[1] Hagel G et al.; doi.org/10.1016/j.annonc.2022.04.347
[2] TICC-1 study: Value of In-vitro testing anti-cancer therapy sensitivity on tumorspheres from patients with metastatic colorectal cancer. Danish
Medicines Agency (EudraCT no. 2017-000456-26) and Regional Committees on Health Ethics for Southern Denmark (S-20170028), University
Hospital Vejle, Denmark. NCT 03251612 https://ascopubs.org/doi/abs/10.1200/JCO.2021.39.15_suppl.e15567
[3] Wensink et al.; npj Precision Oncology (2021) 5:30 ; doi.org/10.1038/s41698-021-00168-1
[4] Grothey A. et al.; CORRECT Study Group. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an
international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013 Jan 26;381(9863):303-12.
[5] Mayer RJ et al.: RECOURSE Study Group. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015 May
14;372(20):1909-19.